
The Next Orbit podcast explores the decisions, tools, and systems behind healthcare data infrastructure through conversations with innovators, data scientists, AI ethicists, and policymakers building the future of interoperability.


AI is like a trash panda designed to solve complex data problems at scale.


Discover how HDUs can transform public health from reactive reporting to predictive infrastructure.

"Good enough" provider data quality is costing plans millions they're not tracking.

.png)
MA plans score 200 points below other industries on digital satisfaction. AI is changing that.

As AI grows, the fate of healthcare data standards like FHIR and USCDI is anything but settled.

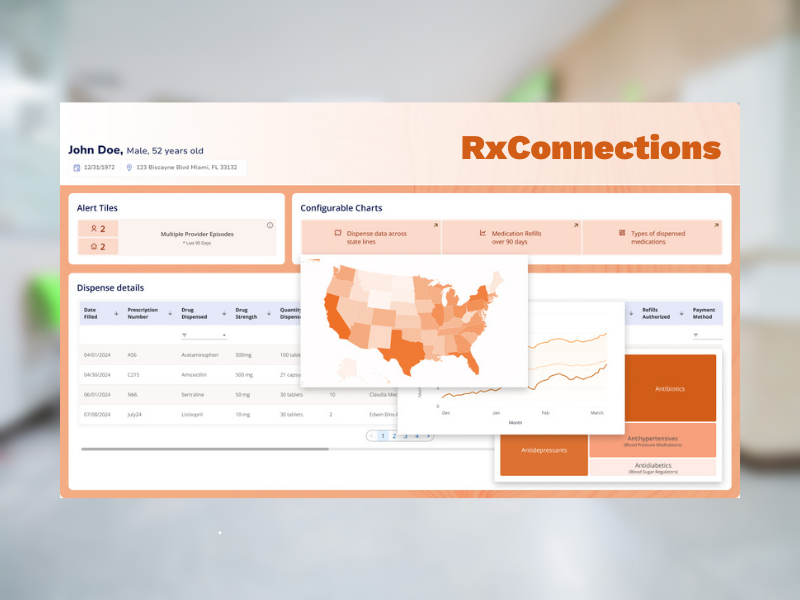
Leap Orbit’s PDMP Access for All pilot gives rural health systems in Kentucky and Illinois a no-cost alternative for integrating mandatory PDMP checks directly into their EHRs.


Everything you need to know about New York’s new behavioral health network adequacy standards.

Manual data entry shouldn’t be part of solving complex deaths. There’s a better way.


New York Health Plan Association analyzed over 300 behavioral health providers across multiple health plans. Find out what was revealed about their network.

.png)
See how provider directories and APIs improve accuracy, compliance, and member experience.


Medicare Advantage plans face mounting pressure to improve Star ratings. The key to unlocking higher scores? Clean, complete, and current provider data.


AI may improve healthcare—but when it starts making decisions about who gets pain relief, we need to ask harder questions.


Learn how to choose a provider data automation partner with this three-step framework.


Leap Orbit isn’t just another health tech company—it’s a company built on curiosity, problem-solving, and a relentless drive to make healthcare better.


Health plans will face new CMS provider directory requirements beginning July 1, 2025.


Learn about what's new and how our solutions help simplify health data interoperability.


TEFCA aims to finally make seamless data exchange in healthcare a reality.


Accreditation is vital to ensure secure, compliant, and quality data exchange processes.


New Brunswick is now at the forefront of Canada’s tech-enabled healthcare ecosystem.


PDMPs should maintain medical ethics, prioritizing patient privacy and delivering comprehensive, bias-free insights.

.png)
EHNAC accreditation is a demonstration of our seriousness about privacy and security.

.png)
CRISP HIE created open-source data solutions that other states’ HIEs can leverage and build upon.


How states and third-party tech providers are uniting against PDMP monopolies.


The U.S. organ transplant system is failing patients due to outdated technology and inefficiencies. With scalable, standards-driven solutions, we have a real opportunity to build a faster, fairer, and more transparent network that saves lives.

.png)
Learn how this community-based care organization went from member frustration to seamless access.


Learn how Maryland's health information exchange solved longstanding provider data challenges.


Convergent helps consumers confidently search for care via the Washington Healthplanfinder.


Leap Orbit announced today that it has re-acquired the RxGov Prescription Drug Monitoring Platform.
